Title: Real-time Visualization and Quantification of Perfusion using Laser Speckle Contrast Imaging in Minimally Invasive and Open Esophagectomies.
Authors: Yao Liu, Garrett Skinner, Lubomyr Boris, Colin Dunn, Chris McCulloh, Peter Kim, Atuhani Burnett, Blair Jobe, Kirsten Newhams
Aims: Esophageal anastomotic leaks are among the most feared in gastrointestinal surgery and are attributed to inadequate tissue perfusion or excess tension. Real-time intraoperative perfusion assessment may identify perfusion deficits to help prevent leaks. Laser Speckle Contrast Imaging (LSCI) provides real-time, repeatable, and on-demand perfusion assessment without dyes, unlike Indocyanine Green fluorescence angiography (ICG-FA). Herein, we report early experience with real-time LSCI quantification of gastric conduit perfusion during esophago-gastric reconstruction.
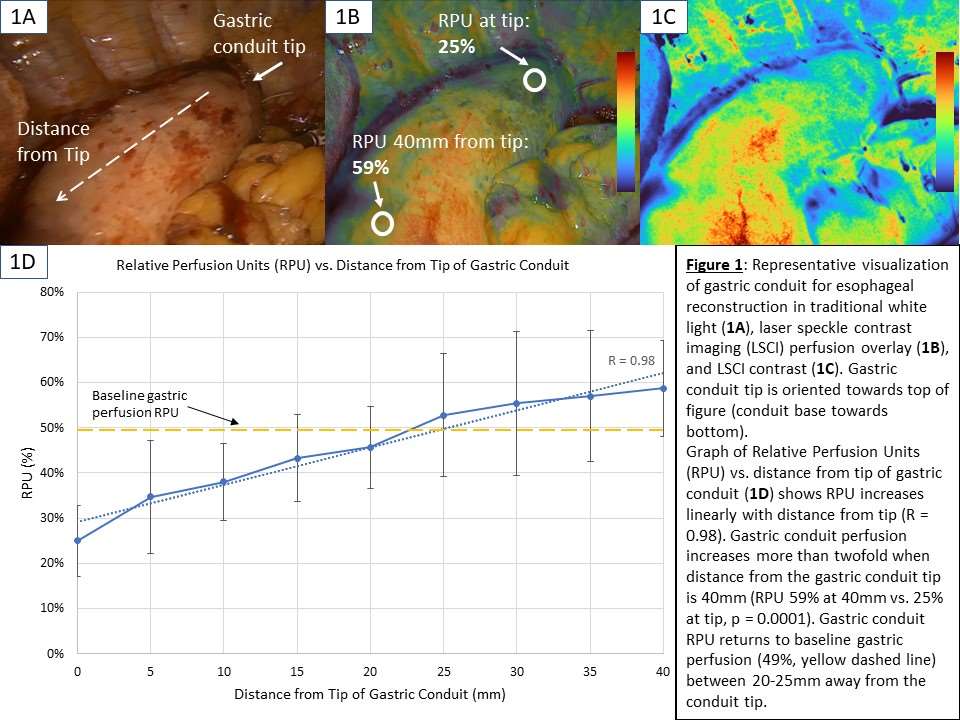
Methods: ActivSightTM (Activ Surgical, Boston, MA) combines LSCI and ICG fluorescence technology in a minimally invasive form factor (FDA-cleared, CE-marked). LSCI detects microvascular blood flow by capturing coherent laser light scatter from red blood cells. A prototype ActivSight feature displays LSCI quantification in relative perfusion units (RPU) compared to reference perfused tissue. 12 consecutive Ivor-Lewis esophagectomies (9 minimally invasive, 3 open) from two US institutions with intraoperative assessment of perfusion in the gastric conduit and esophagogastric anastomoses were analyzed. RPU analysis was performed from the tip of the gastric conduit to 40mm away.
Results: Gastric conduit perfusion changed linearly with increasing distance from the conduit tip (R = 0.98) and demonstrated a more than twofold increase in perfusion from the conduit tip to 40mm proximal (RPU 25% vs 59%, p = 0.0001) (Figure 1D). Gastric conduit perfusion returned to baseline gastric perfusion (49%) 20-25mm distance from the conduit tip. There was one anastomotic leak in this interim analysis of 12 cases (8.3%). Participating surgeons reported clinical decision changes based on LSCI perfusion assessment and a preference of LSCI over ICG-FA due to real-time assessment, repeatable on-demand usability, and workflow improvements.
Conclusions: In this early clinical experience using LSCI, LSCI perfusion quantification displays real-time perfusion gradients with high spatial resolution during esophageal reconstruction. LSCI perfusion information, both color heatmap and quantification, can augment intraoperative decision making in high-risk anastomoses. LSCI shows potential advantages over dye-based perfusion assessment including reproducible and precise visualization of ischemia/perfusion gradient during esophageal resection and reconstruction.